Everyone living with chronic hepatitis B requires initial assessment and then regular monitoring. It is recommended that certain people with hepatitis B undergo hepatocellular carcinoma (HCC or liver cancer) surveillance.
Regular monitoring includes blood tests every 6 months to monitor for progression from one phase of infection to another and determine antiviral treatment eligibility. The natural history of hepatitis B can be divided into 4 progressive phases based on viral load, liver function tests and HBeAg/Ab status. Eligibility for antiviral treatment and specific monitoring is based on the patient’s current disease phase.
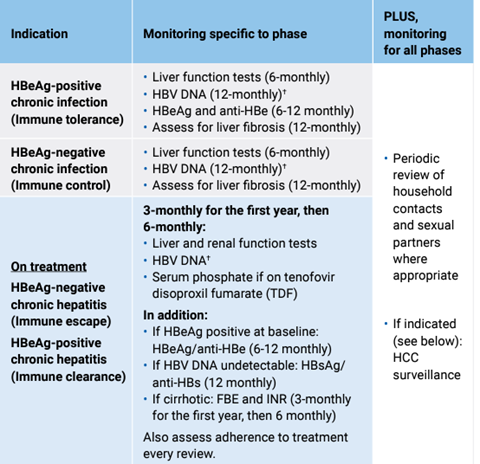
For detailed information on monitoring requirements see the hepatitis B decision making tool.
For information on HCC screening eligibility see here.
Monitoring and/or HCC surveillance can be done by a GP or nurse practitioner, with support and advice from and referral to either a tertiary specialist or hepatitis B s100 prescriber when required.
“The demand on specialist liver services is increasing with the complexity of MASLD-related liver disease, along with other aetiologies of advanced liver disease. Chronic HBV can be effectively managed within primary health, with support from specialist liver centres. Find out who your local HBV-expert is and have them on speed-dial – we are always happy to take phone calls or emails about patients with chronic HBV.” – Liver Nurse | Regional Victoria
Decision making in hepatitis B | PDF| ASHM
B Positive: Clinical assessment of patients with hepatitis B virus infection | Website | ASHM
Australian consensus recommendations for the management of hepatitis B infection | PDF | Gastroenterological Society of Australia
When treatment is indicated, the primary goals are to control viral replication and improve both quality of life and survival by:
B Positive: Treatment of hepatitis B infection | Website | ASHM
In most instances scripts for hepatitis B medications can only be written by an s100 community prescriber or a tertiary specialist/clinician affiliated with a hospital.
For more information on HSD prescriber requirements go to Prescriber eligibility for highly specialised drugs on the Services Australia website.
Community access arrangements | Website | Services Australia
There are some cases in which medication can be discontinued. For example, if a non-cirrhotic patient loses HBsAg irrespective of the development of anti-HBs.
In non-cirrhotic HBeAg-positive patients, who have seroconverted to Anti-HBe positive and have had a HBV DNA VL < 20 IU/mL over a sustained period (e.g. at least two years), stopping therapy can be considered.
These are uncommon circumstances and should be managed by or in collaboration with a tertiary specialist.
People who start medication while pregnant are often recommended to discontinue after birth. For more information on hepatitis B and pregnancy see here.
B Positive: Treatment of chronic hepatitis B virus infection | Website | ASHM
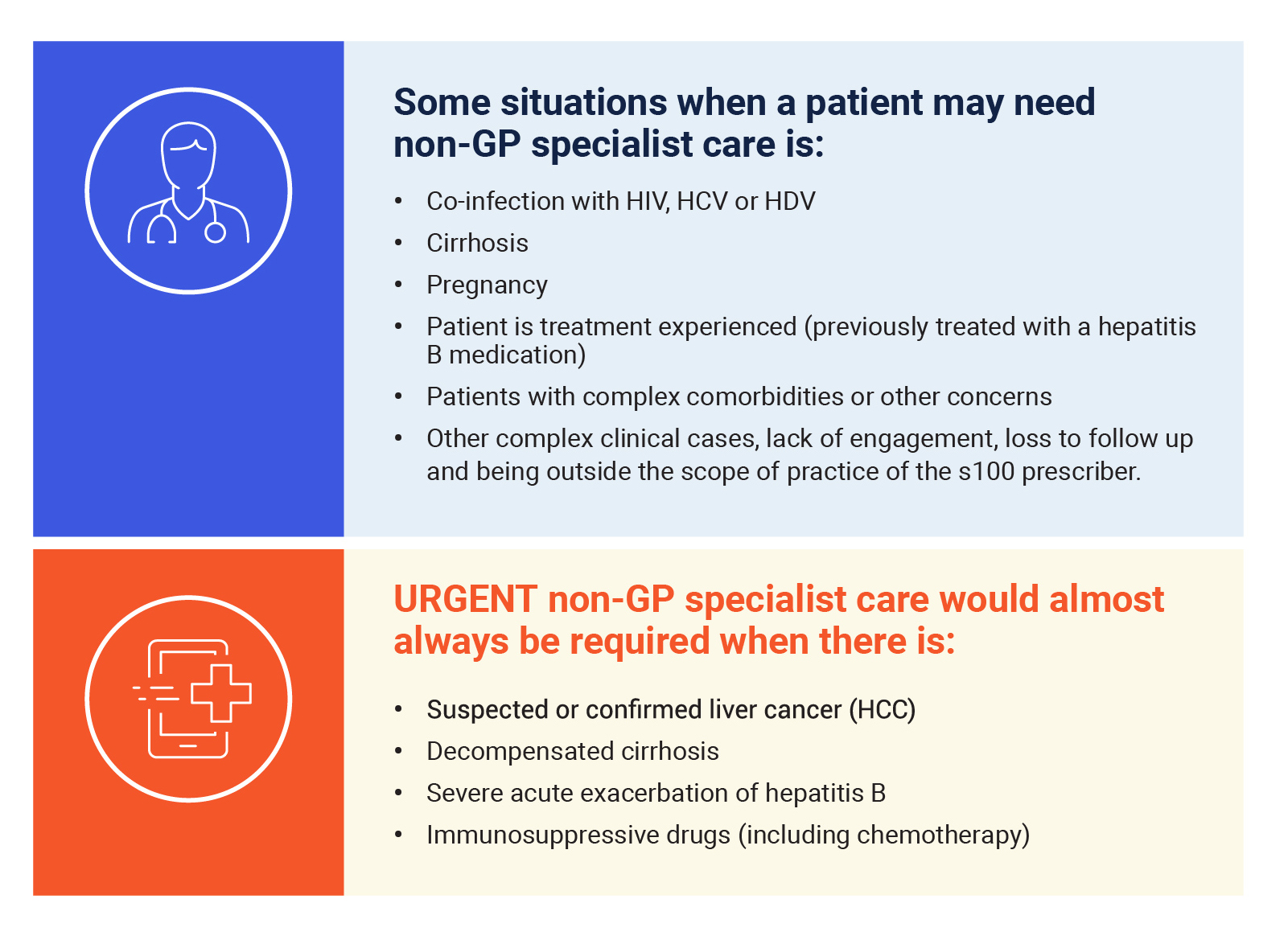
If treatment needs to be initiated, you need to refer your patient to either an accredited GP hepatitis B s100 prescriber in a community setting or a tertiary specialist (such as a liver clinic).
People with cirrhosis and hepatitis B should be referred to a tertiary centre or you should seek advice on management.
Certain situations require referral to a tertiary centre or further advice if geography or wait lists mean referral is not appropriate.
For information on assessing whether or not a person requires medication see the hepatitis B decision making tool.
Medications for hepatitis B on the PBS include entecavir and tenofovir. These can only be initiated and prescribed by an accredited hepatitis B community s100 prescriber or a tertiary specialist.
There is a provision for GPs to prescribe maintenance therapy when it is impractical to get a prescription from the treating affiliated specialist medical practitioner and the specialist has agreed to the prescription. For more information see here.
For information on hepatitis B and pregnancy see here.
Co-infection with HIV, HCV or HDV. For information on co-infection see here.
For guidance on where to refer your patient see here.
Local information regarding referral can be found on HealthPathways. For further information and links to location-specific HealthPathways in Victoria see here.
Hepatitis B referral and clinical support resources | Website & various resources | ASHM
For further training on hepatitis B care options and referrals, complete the Clinical Extensions of Hepatitis B: Care options, monitoring, treatment and referrals module | Online learning module | ASHM
“Whenever I have told a patient that I can manage their hepatitis B in general practice, they have always been really keen to take this up. If they can come and see me, instead of going through the public hospital system, it saves them time and enhances their continuity of care and whole person care.” – Hepatitis B s100 Community Prescribing GP | Melbourne
Whether a referral to a tertiary specialist or an s100 GP is most appropriate depends on your patient’s geographic location, clinical and social situation and other requirements.
Use the Hepatitis B referral options tool to determine the best referral options for your patient. This tool will help you decide whether a primary care referral to an s100 prescriber is appropriate or if a referral to a tertiary specialist is required.
See information on how to complete the referral here.
Hepatitis B referral options tool | Interactive tool | ASHM
Hepatitis B referral and clinical support resources | Website & various resources | ASHM
Referral to an s100 community prescriber
Find a hepatitis B s100 community prescriber here.
Use this referral letter template to initiate the referral.
This roles and responsibilities template and ongoing communication template can also be used to communicate with s100 prescribers.
We suggest making contact with the clinic and/or s100 prescriber before sending the referral.
Referral to a tertiary specialist
In Victoria referral pathways to tertiary specialist differ depending on region. HealthPathways provides localised information. See below for a link to your relevant HealthPathways.

Western Victoria HealthPathways
HealthPathways Melbourne | Eastern Melbourne PHN & North Western Melbourne PHN
“The things that have worked really well over time … are the nurse-led clinics that [the VH outreach nurses] offer … they’re brilliant … they know the patients … they are an amazing resource and support” – Dr Jacqui Richmond | Viral Hepatitis Nurse Consultant | Barwon Public Health Unit and Burnet Institute
Hepatitis B s100 community prescriber map | Website | ASHM
Hepatitis B referral and clinical support resources | Website & various resources | ASHM
It is important to support your patient with information about lifestyle modifications that can improve liver health:
It is important to encourage patients to discuss any complementary or traditional Chinese medicines they may be taking or planning to take as many of these can have an adverse effect on liver health and/or interact with other medications.
Foundation for Alcohol Research and Education | Website
Quit (including Quitline) | Website
Guide for preventative activities in general practice (Red Book) | Website & PDF | RACGP
“My hepatologist told me to see her again when I turn 50. I am 35 now. I almost forgot I was a hep B carrier until wanting to pursue studies in nursing. When I researched online it says to monitor the virus every 6-12 months. I’m confused why my hepatologist didn’t mention this but only to see her again when I’m 50. Does it mean nothing can happen to me in between and I’m ok before then?” – Community member with lived experience of hepatitis B
See below for a list of relevant community resources
Who can give me care for hepatitis B? (multiple languages available) | PDF | Hepatitis Australia
Treatment for hepatitis B & Check-ups for hepatitis B (multiple languages available) | PDF | St Vincent’s Hospital Melbourne
The Hep B Story App | Web-based app | Menzies School of Health Research
The Hepatitis B Story (multiple languages available) | Website & PDF | St Vincent’s Hospital Melbourne
ASHM Head Office - Sydney
Level 3, 160 Clarence Street Sydney, NSW 2000
Tel: (+61) 02 8204 0700
ASHM acknowledges the Traditional Owners of Country across the various lands on which we live and work. We recognise Aboriginal and Torres Strait Islander peoples’ continuing connection to land, water, and community and we pay our respects to Elders past and present. ASHM acknowledges Sovereignty in this country has never been ceded. It always was, and always will be, Aboriginal land.
The information provided on this website and its related websites and guidelines, and the resources made available by ASHM in any format or medium, are for general information purposes only and are not intended as medical advice or as a substitute for consultation with a qualified healthcare professional. While ASHM Health strives to provide accurate and current resources and information, the resources, information and guidelines made available by ASHM Health do not provide personalised medical advice, diagnosis, or treatment. Healthcare professionals should apply their clinical judgment and consider individual circumstances when using this information. To the extent permitted by law, ASHM Health disclaims all liability for any outcomes resulting from reliance on the information provided. For specific medical concerns, please consult a licensed healthcare provider.
ASHM Health | ABN 48 264 545 457 | CFN 17788 | Copyright © 2024 ASHM