Hepatitis C is curable in most people. Hepatitis C treatment in the form of direct-acting antiviral medicines (DAAs) can cure more than 95% of people living with hepatitis C. While the number of people living with hepatitis C is decreasing overall, the cumulative proportion of people living with hepatitis C initiating DAA treatment remains lower than national targets. In the most recent data from the Kirby Institute, during 2022 seven per cent of the people estimated to be living with hepatitis C in Australia at the start of 2022 received DAA therapy.
There are several barriers preventing people living with hepatitis C from receiving treatment and being cured. Geographic location, limited access to healthcare and testing in some settings, and stigma are all factors which prevent people from receiving treatment.
The NSW Hepatitis C Remote Prescribing program removes some of these barriers, enabling greater access to hepatitis C screening and treatment in New South Wales. Since 2020, the program has increased access to hepatitis C treatment throughout the state through remote prescriptions and patient-centred service delivery facilitated by referring nurses and prescribers.
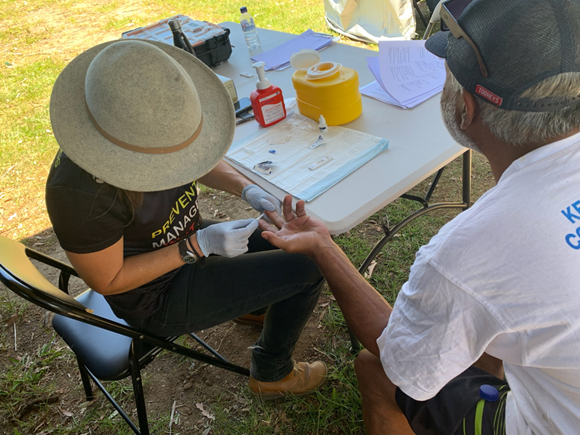
The referring nurses work across a variety of settings which traditionally face increased barriers to hepatitis C testing and treatment. These include alcohol and other drug settings, Aboriginal Community Controlled Health Services, healthcare clinics with limited access to a prescriber, mental health sevices, and community correctional settings. Some referring nurses also use Mobile Health Vans equipped with hepatitis C screening equipment to reach people in regional areas or experiencing homelessness, while providing a stigma-free, private environment.
“Accessing treatment just needs to be easy,” says Jana Van-Der-Jagt, a hepatology nurse practitioner and co-lead of the NSW Hepatitis C Remote Prescriber Program. “The cohort that we’re helping has so many barriers and so many other priorities. For us as healthcare workers, we are aware from our public health point of view that we have this opportunity to eliminate hepatitis C, which is a really just a golden opportunity.”
“We have all the tools that we need to make that happen.”
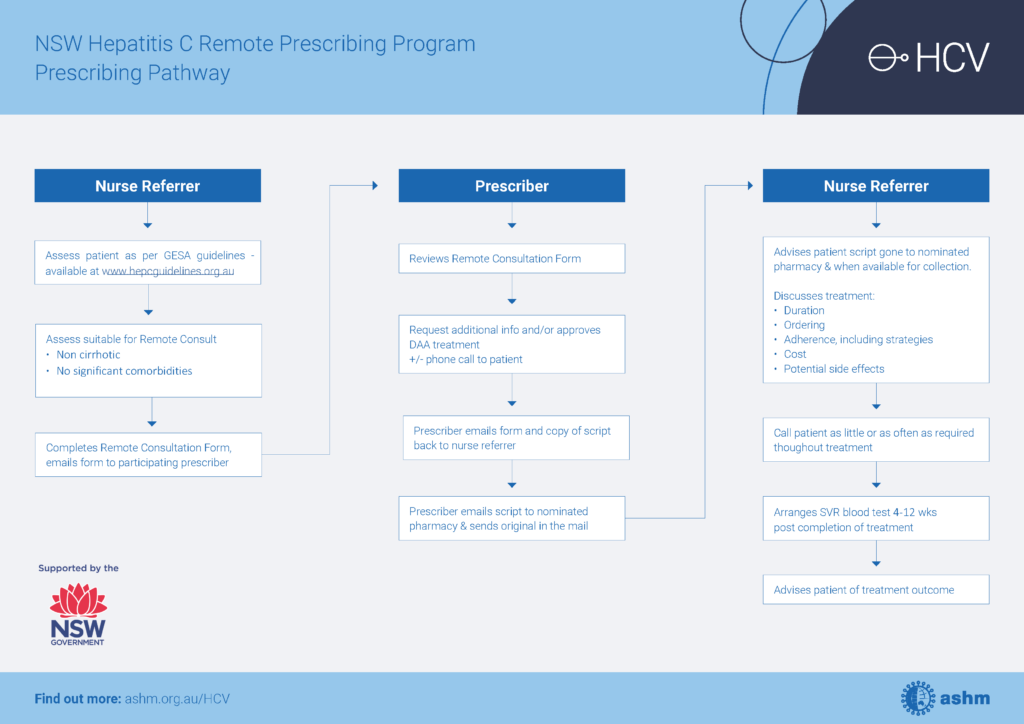
The program helps remove barriers to treatment through its ‘nurse referrers’, who reach out to communities with limited access to hepatitis C treatment prescribers to perform an initial assessment of clients. If the client is suitable for remote prescription, the nurse will refer the details to a participating prescriber who reviews the information and initiates DAA therapy.
Nurse referrers then take a hands-on role to ensure clients have what they need to adhere to treatment and achieve a sustained virologic response (SVR) — that is, no detection of hepatitis C in blood 4 to 12 weeks after treatment completion. Jana explains that these services are person-centred and tailored to the circumstances of each client.
“The nurses will be able to facilitate whatever level of support that the client wants or needs,” says Jana. “Some nurses store clients’ medications for them and meet them in a park once a week, for example.”
Daryl’s Story
Daryl* is a 46-year-old man with unstable housing who was linked with drug & alcohol services. In January 2022, he tested HCV RNA positive. Daryl was referred for remote consultation and commenced treatment in February 2022. The second month’s supply of medication was lost when he was displaced by a natural disaster. Daryl engaged with a nurse referrer who contacted the remote prescriber, and a new prescription was sent to the local pharmacy. The medication was taken to him in the park where he was sleeping and he continued on treatment. In January 2023, Daryl was tested and had achieved SVR.
*Name changed to protect anonymity.
Jana says the nurse-led model of the program is cost-effective and allows nurses to build trust and understand their clients and their needs.
“It’s lovely for nurses to be able to manage the entire episode of care from meeting the patient, building that rapport, doing the assessment, doing the treatment, and doing the follow up. It’s just something that fits beautifully with the nurse-led model,” says Jana.
As of July 2024, the program has helped more than 300 people to be initiated onto treatment. Interim data from a selection of participants taken between 2020 and 2022 shows that the program has been effective in encouraging adherence to treatment, with 28 out of 30 clients (93%) achieving SVR following their remote prescriber-initiated treatment.
”There are hundreds and hundreds of people who have been treated, who otherwise would not have been treated. I think the program is making a difference and it’s exciting to be part of building that momentum,” says Jana.
Medical practitioners, authorised nurse practitioners and nurses interested in finding out more about the program and how to join can access NSW Hepatitis C Remote Prescribing Program webpage.
The NSW Hepatitis C Remote Prescribing Program is funded by NSW Health and coordinated by ASHM.