Women living with HIV often have complex intersecting medical and psychosocial needs. The HIV Monitoring Tool for Women promotes an integrated, holistic, women-centered approach to providing HIV care for women in Australia.
Women living with HIV experience greater multimorbidity at a younger age than men living with HIV, with most of these comorbidities carrying a higher mortality risk, according to one review of the ATHENA cohort. Moreover, women living with HIV are disproportionately affected by intimate partner violence and experience higher rates of mental health conditions such as depression and anxiety.
Despite the experience of cisgender women living with HIV varying greatly from other populations in Australia, there is currently a lack of standardised guidance for managing the health of women living with HIV, with current standards of care often overlooking the unique needs of women living with HIV.
This was one of the findings at RPA Sexual Health, where team members ran an audit of the routine HIV care services provided to cisgender women living with HIV at their clinic. Key co-morbidity screenings for ageing women (bone mineral density scan, fracture risk assessment score, and cognitive screening) were not performed for any patients aged over 45 years in the prior 12 months. Only 30% of women were screened for domestic and family violence. The study also identified a “lack of routine menopause screening and discussion with patients, which is not uncommon among HIV clinicians and other healthcare providers”. Since then, RPA Sexual Health has taken successful steps to address these gaps in their practice.
However, action towards more comprehensive HIV care for women extends far wider than just the RPA Sexual Health clinic – it’s a national problem to address.
To facilitate better outcomes for women living with HIV, ASHM has worked with members of the RPA Sexual Health team and clinical advisors to launch a comprehensive reference tool for healthcare providers managing the care of cisgender women living with HIV.
The HIV Monitoring Tool for Women* is a quick reference tool with links to relevant clinical tools and guidelines. It utilises a holistic, women-centered approach to HIV monitoring and care tailored to cisgender women living with HIV – particularly aging women.
Ageing women living with HIV face a higher burden of cardiovascular disease, mental health conditions, and reduced bone mineral density compared to HIV-negative women. These are all compounded by the fact that women living with HIV may be more likely to experience menopause earlier and with more severe menopausal symptoms, potentially negatively affecting quality of life and engagement with HIV care. With an estimated 50% of women living in Australia being over the age of 40 as of 2021, it is critical that healthcare professionals are informed and confident managing the unique needs of aging women living with HIV.
The HIV Monitoring Tool for Women provides guidance on the often overlook co-morbidities of women living with HIV and encourages proactive health management by incorporating screening questions and resources around menopause, sexual and reproductive health, mental and cognitive health, psychosocial issues (including domestic and family violence and substance use), and common conditions associated with ageing.
Dr Rachel Burdon, Senior Staff Specialist and Deputy Director of RPA Sexual Health and a key clinical advisor on the HIV Monitoring Tool for Women, explains that the tool considers HIV management alongside other health and psychosocial issues that may impact women.
“If you silo HIV management from all the other health and psychosocial needs of women living with HIV, you’re never going to get good outcomes because they all these issues intersect and interact with each other,” says Dr Burdon.
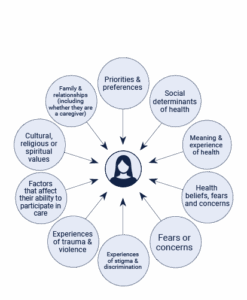
The additional conditions that women living with HIV face are not just medical. Dr Burdon notes that the psychosocial determinants of health including social isolation and vulnerability, concerns regarding finances and visa status, caring for immediate and extended family, disclosure and stigma, substance use, domestic and family violence, visa status and access to Medicare, a can all impact negatively on women living with HIV, affecting their adherence to monitoring, access to care, and ultimately, health outcomes.
“In 2025 HIV care should not be solely focused on managing the virus and achieving an undetectable viral load,” says Dr Burdon. “Managing women’s holistic health needs and providing proactive preventive care is really important. Recognising and addressing the psychosocial context in which women living with HIV exist outside of the clinic is really, really critical. Providing holistic women centered care improves health outcomes, supports adherence and retention in care and addresses the priorities of our patients.”
The HIV Monitoring Tool for Women incorporates social and environmental determinants of health and sexual and reproductive health as key components of HIV monitoring. The easy-to-understand reference tool prompts clinicians to listen and understand patients’ priorities and circumstances, addressing factors such as finances, cultural backgrounds and norms, domestic and family violence, social support systems, and more.
"Last week I saw one of our regular patients who is a WLHIV and been attending our clinic for many years. She keeps repeating that she couldn’t believe how much our care has changed her life. Since we started being more proactive with screening and management as a result of the audit, she says she has never felt healthier or happier – she is in charge of her life and her health."
- Dr Burdon, on how the changes to their practice towards incorporating a more comprehensive approach to HIV care has impacted one of their patients.
While the tool is comprehensive in its scope, Dr Burdon says that it is designed to be highly flexible and realistic.
“[In my practice], we’re only seeing people every six months to one year, and there’s a limit on what you can do in one consult,” says Dr Burdon.
“All of the additional conditions and issues mentioned in the tool aren’t going to apply to all women living with HIV. Instead, the tool should be used as a checklist – to help prioritise triage issues that the patient and clinician identify as needing to be addressed with the aim of developing a care plan to manage them. It’s impossible to address all issues in a single visit or at every visit.”
By using the tool with a women-centred, integrated approach, clinicians can ensure they can confidently address the unique needs of women living with HIV.
The HIV Monitoring Tool for Women is available on the ASHM website: https://ashm.org.au/resources/hiv-monitoring-tool-for-women/
*Note: The term ‘women’ and ‘woman’ is used throughout this article and the HIV Monitoring Tool for Women to refer to cisgender women specifically. However, ASHM recognises that “woman”/”women” and “female” also includes non-binary, gender diverse, and transgender women. Information and clinical guidance for non-binary, gender diverse and transgender women living with HIV can be found in other guidelines and resources, such as the ASHM HIV Management Guidelines: Transgender People Living with HIV.

