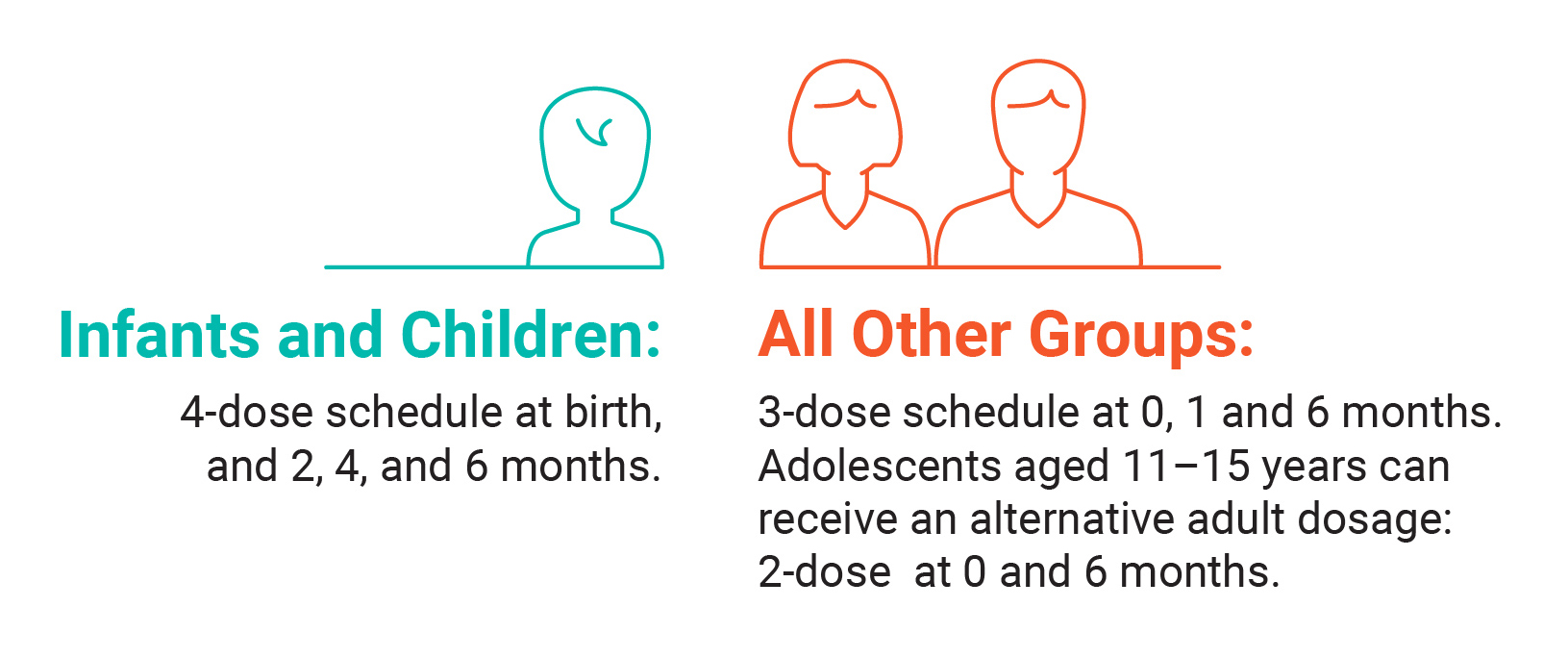
Hepatitis B vaccination is recommended for the following groups of people.
Hepatitis B | The Australian Immunisation Handbook | Website | Australian Government Department of Health and Aged Care
Hepatitis B vaccine | Website | Australian Government Department of Health and Aged Care
National Immunisation Program and state-funded vaccines for eligible Victorian adults | Website | Victorian Government Department of Health
B Positive: Primary prevention of hepatitis B infection | Website | ASHM
Hepatitis B | The Australian Immunisation Handbook | Website | Australian Government Department of Health and Aged Care
Catch up vaccination | Website | Australian Government Department of Health and Aged Care
This is a comprehensive fact sheet on hepatitis B disease and vaccines: Hepatitis B vaccines for Australians | PDF | National Centre for Immunisation Research and Surveillance
B Positive: Primary prevention of hepatitis B infection | Website | ASHM
Catch-up immunisation in refugees | Website | Royal Children’s Hospital Melbourne
For people at imminent risk of exposure to hepatitis B an accelerated vaccination schedule is available. For information on dose, vaccine, age of recipient, recommended schedule and minimum intervals, see here.
Accelerated hepatitis B vaccination schedules for people with imminent risk of exposure | Website | Australian Government Department of Health and Aged Care
It depends. Serological testing may be warranted for some adolescents and adults without evidence of previous vaccination, particularly those at increased risk, who would usually be indicated for testing.
Hepatitis B vaccination is free for Medicare-eligible people when administered as per the National Immunisation Program schedule (at birth, 2, 4 and 6 months). Catch up hepatitis B vaccination is also funded for people under 20 years of age.
Refugee and humanitarian entrants are eligible for these funded vaccines if missed in childhood.
The Victorian Government also funds routine and catch-up hepatitis B vaccine where clinically indicated including for:
If cost is a barrier and a person is eligible for funded vaccination they may be able to access this for free at bulk-billing clinics, community health services or sexual health clinics.
The inclusion of Aboriginal peoples as a priority for vaccination highlights the enduring traumatic legacy of colonisation, recognising the historical disadvantage perpetuated by institutional racism and systemic failures that collectively contribute to health disparities between Aboriginal peoples and non-Indigenous Australians.
Immunisation schedule Victoria and vaccine eligibility criteria | Website | Victorian Government Department of Health
National Immunisation Program Schedule | Website | Australian Government Department of Health and Aged Care
Order form for funded vaccine| Online Form | Onelink Australia
Performing hepatitis B serology following hepatitis B vaccination is not routinely indicated.
Post-vaccination screening, is recommended for:
This should be completed 4 weeks after the final vaccine dose.
If there is a current Anti-HBs level of < 10 mlU/mL 4–8 weeks following the final vaccine dose with a documented age-appropriate vaccine history, the person is deemed a non-responder. In this instance, you should follow the pathway provided here.
If a non-response persists, the patient should be informed of their immune status and advised to minimise exposures. If exposed, hepatitis B immunoglobulin can be given within 72 hours.
People living with hepatitis B often have questions about transmission risk and how to reduce this.
Give additional advice to prevent transmission: avoid sharing sharp items (eg razor, toothbrush, nail clipper, earrings), cover open cuts or skin wounds and clean blood or body fluid spilled onto surfaces with bleach.
When diagnosed as part of antenatal screening, pregnant people may have concerns and questions about vertical transmission. See further information on hepatitis B and pregnancy here.
It is important to ensure your patient understands the following:
Australian consensus recommendations for the management of hepatitis B infection | PDF | Gastroenterological Society of Australia
For further training on hepatitis B transmission and prevention, complete the Clinical Extensions of Hepatitis B: Transmission and Natural history module | Online learning module | ASHM
No. Clinicians and healthcare workers should follow standard infection control procedures for all people. These are adequate to prevent hepatitis B transmission.
No further precautions are required beyond these standard precautions when you are providing care for someone living with a blood-borne virus, including hepatitis B. Ineffective and unnecessary methods such as double gloving, wearing gowns or placing a person last on a consult list only perpetuate stigma and discrimination. This can negatively impact a person’s wellbeing and result in reduced engagement in healthcare.
Healthcare workers should be vaccinated and aware of their vaccination and immune status.
B Positive: Infection control and occupational health | Website | ASHM
Australian Guidelines for the Prevention and Control of Infection in Healthcare | PDF | National Health and Medical Research Council
“They say Hepatitis B is contagious, so I thought I had to stop sharing utensils with family members to protect them.” – Community member with lived experience of hepatitis B
“I was too scared to tell my partner about having hepatitis B. What if he thought I’d been unfaithful and stopped loving me?” – Community member with lived experience of hepatitis B
See below for a list of relevant community resources
Hepatitis B immunisation | Website | Better Health Channel
Hepatitis B vaccination | Website | Hepatitis Australia
Hepatitis B and relationships | Website | Hepatitis Australia
This plain English resource is designed to support health workers discussing chronic hepatitis B with patients, including refugee and migrant communities: The Hepatitis B Story (multiple languages available) | Website & PDF | St Vincent’s Hospital Melbourne
Hepatitis B: It’s family business (multiple languages available) | Website | Multicultural HIV and Hepatitis Service
ASHM Head Office - Sydney
Level 3, 160 Clarence Street Sydney, NSW 2000
Tel: (+61) 02 8204 0700
ASHM acknowledges the Traditional Owners of Country across the various lands on which we live and work. We recognise Aboriginal and Torres Strait Islander peoples’ continuing connection to land, water, and community and we pay our respects to Elders past and present. ASHM acknowledges Sovereignty in this country has never been ceded. It always was, and always will be, Aboriginal land.
The information provided on this website and its related websites and guidelines, and the resources made available by ASHM in any format or medium, are for general information purposes only and are not intended as medical advice or as a substitute for consultation with a qualified healthcare professional. While ASHM Health strives to provide accurate and current resources and information, the resources, information and guidelines made available by ASHM Health do not provide personalised medical advice, diagnosis, or treatment. Healthcare professionals should apply their clinical judgment and consider individual circumstances when using this information. To the extent permitted by law, ASHM Health disclaims all liability for any outcomes resulting from reliance on the information provided. For specific medical concerns, please consult a licensed healthcare provider.
ASHM Health | ABN 48 264 545 457 | CFN 17788 | Copyright © 2024 ASHM