
When studying the genotype of chronic hepatitis B (CHB) in the Northern Territory (NT), researchers discovered that 100% of CHB in Aboriginal and Torres Strait Islander peoples in the NT is due to the unique sub-genotype C4 , which is associated with quicker progression to liver cancer and cirrhosis.
“It upped the urgency for us to try to work towards the elimination of chronic hepatitis B as a public health problem within the Northern Territory,” says Associate Professor Jane Davies, a Clinical Researcher at Menzies School of Health Research (Menzies) involved in the research.
In response, the idea for Hep B PAST was formed with the goal of sustainably eliminating chronic hepatitis B in the NT. The project is a collaboration between Menzies, ASHM, Northern Territory Government, Miwatj Health Aboriginal Corporation, the Katherine West Health Board, and NT AIDS and Hepatitis Council (NTAHC), alongside community stakeholders.
“We came together to try to look at this from a holistic – both clinical and research – perspective and involve people living with chronic hepatitis B and the Aboriginal health workforce within the NT and to try to put together a plan,” says Jane.
Following four years of development, the project received funding from the National Health and Medical Research Council in 2018. Since then, Hep B PAST has evolved into a multi-faceted project covering hepatitis case-finding, workforce training, and in-language public education. You can read about each part of Hep B PAST below.
The first step of Hep B PAST was determining the hepatitis B status of participating Aboriginal and Torres Strait Islander peoples in the NT. Community feedback advised against further blood tests unless necessary. Hep B PAST instead used previous blood test and vaccination data from several electronic health record systems to determine the hepatitis B status of around 40,000 people, or approximately 60%, of the Aboriginal and Torres Strait Islander population in the NT. Participants living with hepatitis B were then allocated a care pathway and linked to appropriate services.
By identifying the geographic prevalence of hepatitis B throughout Aboriginal and Torres Strait Islander communities in the NT, the Hep B PAST team were also able to assess where to direct trained clinical care teams and resources to deliver services such as Fibroscans®.
Sources:
Hosking K, et al. Evaluating a novel model of hepatitis B care, Hep B PAST, in the Northern Territory of Australia: results from a prospective, population-based study, The Lancet Regional Health – Western Pacific, Volume 48, 2024, 101116, ISSN 2666-6065, https://doi.org/10.1016/j.lanwpc.2024.101116
After identifying a gap in chronic hepatitis B training for the Aboriginal and Torres Strait Islander health workforce in the NT, the Hep B PAST team worked closely with Aboriginal Health Practitioners to co-design course materials, training, and evaluation tools for the ‘Managing Hepatitis B’ course.
The 1.5-day interactive course enhances Aboriginal and Torres Strait Islander health workforce members’ knowledge and attitudes around hepatitis B prevention, transmission, and management, with training delivery focusing on two-way communication, cultural safety, respect, and empowerment.
So far, the course has been delivered to over 150 Aboriginal health workforce members across the NT, with feedback calling it “the most culturally safe training I’ve ever had.”
Sources:
Hosking, K., De Santis, T., Vintour-Cesar, E. et al. “The most culturally safe training I’ve ever had”: the co-design of a culturally safe Managing hepatitis B training course with and for the Aboriginal health workforce of the Northern Territory of Australia. BMC Health Serv Res 23, 935 (2023). https://doi.org/10.1186/s12913-023-09902-w
Hosking K, De Santis T, Vintour-Cesar E, et al. “Putting the power back into community”: A mixed methods evaluation of a chronic hepatitis B training course for the Aboriginal health workforce of Australia’s Northern Territory. PLoS One. 2024;19(1):e0288577. Published 2024 Jan 24. doi:10.1371/journal.pone.0288577
To increase public knowledge around hepatitis B, Hep B PAST included the translation of the Hep B Story smartphone app into an additional 10 Aboriginal languages.
The Hep B Story app initially launched in 2014 in English and Yolŋu matha, and contained information for people living with hepatitis B and their families around the transmission, progression, and treatment of the virus.
The translation project was co-led by an Aboriginal researcher, and consisted of consultation and collaboration with community members, Elders, Aboriginal Health Practitioners, and translators from each language group.
In adapting the app, the project team ensured the cultural relevancy and appropriateness for each language group and adapted the content as needed. For example, changing a story revolving around fishing to a story around wood collecting for central communities where fishing is uncommon.
The Hep B Story app is now available in English, Yolŋu matha, Kunwinjku, Tiwi, Arrernte, Warlpiri, Pitjantjatjara, Burarra, Anindilyakwa, and Kriol.
Sources:
Binks P, Ross C, Gurruwiwi GG, Wurrawilya S, Alley T, Bukulatjpi SM, et al. Adapting and translating the ‘Hep B Story’ App the right way: A transferable toolkit to develop health resources with, and for, Aboriginal people. Health Promot J Austral. 2024. https://doi.org/10.1002/hpja.858
Binks, P., Venkatesan, S., Everitt, A. et al. An evaluation and refinement of the “Hep B Story” app, tailored to meet the community’s cultural needs. BMC Health Serv Res 24, 710 (2024). https://doi.org/10.1186/s12913-024-11149-y
Between 2018 and 2023, the Hep B PAST project reached more than 40,500 people and involved 66 remote community clinics across the NT. Over this period, the cascade of care for participating Aboriginal and Torres Strait Islander peoples living with hepatitis B improved significantly, far surpassing national elimination targets. At the conclusion of Hep B PAST, an estimated 99.9% of people living with chronic hepatitis B in the study were diagnosed (up from 60.7% pre-Hep B PAST), and 86.3% were engaged in care (up from 13.6% in 2020).
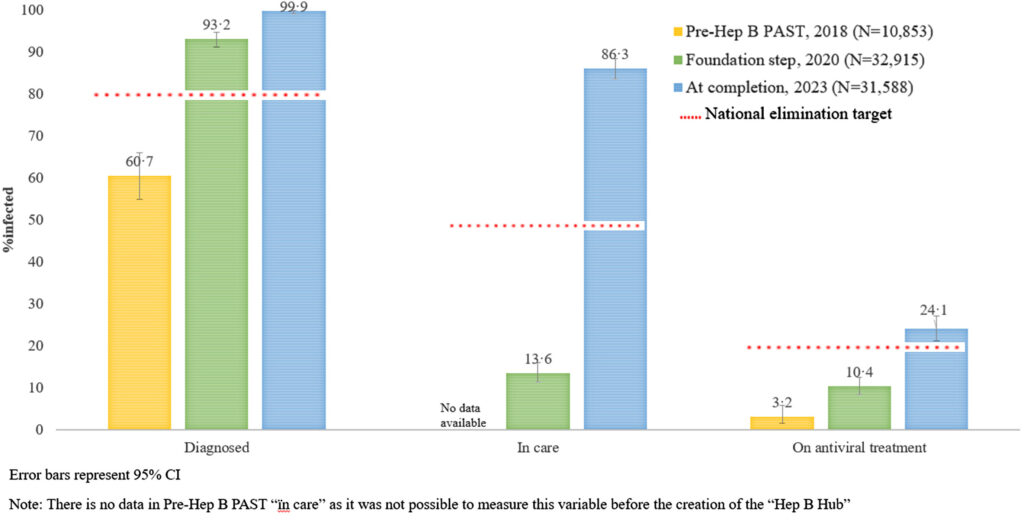
Cascade of care of the study population comparing time points 1. Pre-Hep B PAST (2018), 2. Foundation step (2020), and 3. Completion of Hep B PAST (2023).
Source: Hosking K, et al. Evaluating a novel model of hepatitis B care, Hep B PAST, in the Northern Territory of Australia: results from a prospective, population-based study, The Lancet Regional Health – Western Pacific, Volume 48, 2024, 101116, ISSN 2666-065, https://doi.org/10.1016/j.lanwpc.2024.101116
Co-design and partnership vital to success

Members of the Hep B PAST project team say the key to its success is its participatory action research approach built upon co-design, cultural safety, and respect.
Since Hep B PAST’s beginnings in 2014, an Indigenous Reference Group has guided the development of the project, providing feedback and connecting the research team to different communities.
Throughout the development and rollout of all aspects of Hep B PAST, co-design and a sense of shared ownership was central. Dr Kelly Hosking, Director of Sexual Health and Blood Borne Viruses at Northern Territory Government and a Hep B PAST project member, explains how the project’s reciprocal, respect-based approach and “flattening hierarchies” were vital to the success of Hep B PAST’s Aboriginal workforce capacity building training.
“We worked with our Aboriginal Health Practitioners to co-design a course. As part of an iterative, two-way learning process, the community and the course participants also helped shape the course ” says Kelly. “[This resulted in] ownership and empowerment.”
“[The capacity training] is a very two-way learning process using decolonising pedagogies and has had some really great outcomes.”
The course led to a sustained improvement in the knowledge and attitudes of the Aboriginal health workforce, resulting in improved care and treatment uptake for people living with CHB. Course participants also saw improvement in important non-clinical outcomes, including strengthening teaching and leadership skills, and empowerment.
To ensure inclusion in the co-design process, Jane says that working flexibly and adapting as needed were ” key to the success of Hep B PAST and enabling people to be part of it, even if they couldn’t necessarily meet a very strict set of criteria and timelines.”
“We needed to respect the fact that things need to go at the pace that they need to go at for that particular service, community, or group, and that your superimposed Western biomedical timeline is not necessarily appropriate or going to get you the best outcome.”
Creating culturally safe spaces

This consideration for cultural nuances and the personal circumstances of participants extended into every aspect of how the project was delivered.
These measures included ensuring participants are comfortable, integrating storytelling and in-language Hep B Story resources into training, and creating safe spaces by respecting kinship and gender protocols.
“We make sure everyone is okay to be in the same room together,” says Tammy Fernandes, RN and Clinical Coordinator for the Hep B PAST. ” We make sure that we talk about male and female issues separately or we discuss with the group to see how they feel about it, because each group is different.”
The future of Hep B PAST
As Hep B PAST enters its next phase, the project has big ambitions.
Enhancing the clinical capabilities of the program is a priority, particularly introducing point-of-care testing to enable real-time results and conversations about people’s health.
There are also plans for expansion. The project team hopes to expand Hep B PAST to the remaining Aboriginal and Torres Strait Islander population in Northern Territory and interstate to areas such as Far North Queensland.
The potential of Hep B PAST is not just limited to Australia. The program and its approach could drive global progress towards the virtual elimination of hepatitis B.
“We would like to see Hep B PAST adapted and rolled out to a broader range of people across Australia, other culturally and diverse groups, and potentially overseas,” says Jane.
“We think it’s a pretty solid model that could be adapted and replicated for other people to try to move the world towards elimination.”
Darwin image credit: Tourism NT/Shaana McNaught

